Ebola virus disease (EVD) or Ebola hemorrhagic fever (EHF) is the human disease which may be caused by any of four of the five known ebola viruses. These four viruses are: Bundibugyo virus (BDBV), Ebola virus (EBOV), Sudan virus (SUDV), and Taï Forest virus (TAFV, formerly and more commonly Côte d'Ivoire Ebola virus (Ivory Coast Ebolavirus, CIEBOV)). EVD is a viral hemorrhagic fever (VHF), and is clinically nearly indistinguishable from Marburg virus disease (MVD).
Symptoms :
EVD/EHF is clinically indistinguishable from Marburg virus disease (MVD), and it can also easily be confused with many other diseases prevalent in Equatorial Africa, such as other viral hemorrhagic fevers, falciparum malaria, typhoid fever, shigellosis, rickettsial diseases, cholera, gram-negative septicemia or EHEC enteritis. The most detailed studies on the frequency, onset, and duration of EVD clinical signs and symptoms were performed during the 1995 outbreak in Kikwit, Zaire (EBOV) and the 2007–2008 outbreak in Bundibugyo, Uganda (BDBV). The mean incubation period, best calculated currently for EVD outbreaks due to EBOV infection, is 12.7 days (standard deviation = 4.3 days), but can be as long as 25 days. EVD begins with a sudden onset of an influenza-like stage characterized by general malaise, fever with chills, arthralgia and myalgia, and chest pain. Nausea is accompanied by abdominal pain, anorexia, diarrhea, and vomiting. Respiratory tract involvement is characterized by pharyngitis with sore throat, cough, dyspnea, and hiccups. The central nervous system is affected as judged by the development of severe headaches, agitation, confusion, fatigue, depression, seizures, and sometimes coma.
Cutaneous presentation may include: maculopapular rash, petechiae, purpura, ecchymoses, and hematomas (especially around needle injection sites). Development of hemorrhagic symptoms is generally indicative of a negative prognosis. However, contrary to popular belief, hemorrhage does not lead to hypovolemia and is not the cause of death (total blood loss is low except during labor). Instead, death occurs due to multiple organ dysfunction syndrome (MODS) due to fluid redistribution, hypotension, disseminated intravascular coagulation, and focal tissue necroses.
Treatment:
There is currently no FDA-approved ebolavirus-specific therapy for EVD. Treatment is primarily supportive in nature and includes minimizing invasive procedures, balancing fluids and electrolytes to counter dehydration, administration of anticoagulants early in infection to prevent or control disseminated intravascular coagulation, administration of procoagulants late in infection to control hemorrhaging, maintaining oxygen levels, pain management, and administration of antibiotics or antimycotics to treat secondary infections. Hyperimmune equine immunoglobulin raised against EBOV has been used in Russia to treat a laboratory worker who accidentally infected herself with EBOV—but the patient died anyway. Experimentally, recombinant vesicular stomatitis Indiana virus (VSIV) expressing the glycoprotein of EBOV or SUDV has been used successfully in nonhuman primate models as post-exposure prophylaxis. Such a recombinant post-exposure vaccine was also used to treat a German researcher who accidentally pricked herself with a possibly EBOV-contaminated needle. Treatment might have been successful as she survived. However, actual EBOV infection could never be demonstrated without a doubt. Novel, very promising, experimental therapeutic regimens rely on antisense technology. Both small interfering RNAs (siRNAs) and phosphorodiamidate morpholino oligomers (PMOs) targeting the EBOV genome could prevent disease in nonhuman primates.
Referal sources and evidences of this disease:
The above video is about ebola virus outbreak .
Case studies
Symptoms :
EVD/EHF is clinically indistinguishable from Marburg virus disease (MVD), and it can also easily be confused with many other diseases prevalent in Equatorial Africa, such as other viral hemorrhagic fevers, falciparum malaria, typhoid fever, shigellosis, rickettsial diseases, cholera, gram-negative septicemia or EHEC enteritis. The most detailed studies on the frequency, onset, and duration of EVD clinical signs and symptoms were performed during the 1995 outbreak in Kikwit, Zaire (EBOV) and the 2007–2008 outbreak in Bundibugyo, Uganda (BDBV). The mean incubation period, best calculated currently for EVD outbreaks due to EBOV infection, is 12.7 days (standard deviation = 4.3 days), but can be as long as 25 days. EVD begins with a sudden onset of an influenza-like stage characterized by general malaise, fever with chills, arthralgia and myalgia, and chest pain. Nausea is accompanied by abdominal pain, anorexia, diarrhea, and vomiting. Respiratory tract involvement is characterized by pharyngitis with sore throat, cough, dyspnea, and hiccups. The central nervous system is affected as judged by the development of severe headaches, agitation, confusion, fatigue, depression, seizures, and sometimes coma.
Cutaneous presentation may include: maculopapular rash, petechiae, purpura, ecchymoses, and hematomas (especially around needle injection sites). Development of hemorrhagic symptoms is generally indicative of a negative prognosis. However, contrary to popular belief, hemorrhage does not lead to hypovolemia and is not the cause of death (total blood loss is low except during labor). Instead, death occurs due to multiple organ dysfunction syndrome (MODS) due to fluid redistribution, hypotension, disseminated intravascular coagulation, and focal tissue necroses.
Treatment:
There is currently no FDA-approved ebolavirus-specific therapy for EVD. Treatment is primarily supportive in nature and includes minimizing invasive procedures, balancing fluids and electrolytes to counter dehydration, administration of anticoagulants early in infection to prevent or control disseminated intravascular coagulation, administration of procoagulants late in infection to control hemorrhaging, maintaining oxygen levels, pain management, and administration of antibiotics or antimycotics to treat secondary infections. Hyperimmune equine immunoglobulin raised against EBOV has been used in Russia to treat a laboratory worker who accidentally infected herself with EBOV—but the patient died anyway. Experimentally, recombinant vesicular stomatitis Indiana virus (VSIV) expressing the glycoprotein of EBOV or SUDV has been used successfully in nonhuman primate models as post-exposure prophylaxis. Such a recombinant post-exposure vaccine was also used to treat a German researcher who accidentally pricked herself with a possibly EBOV-contaminated needle. Treatment might have been successful as she survived. However, actual EBOV infection could never be demonstrated without a doubt. Novel, very promising, experimental therapeutic regimens rely on antisense technology. Both small interfering RNAs (siRNAs) and phosphorodiamidate morpholino oligomers (PMOs) targeting the EBOV genome could prevent disease in nonhuman primates.
Referal sources and evidences of this disease:
Case studies
Unrecognized Ebola Hemorrhagic Fever at
Mosango Hospital during the 1995
Epidemic in Kikwit, Democratic Republic
of the Congo:
On April 20, 1995, a 70-year-old nun, working
as a nurse in Kikwit General Hospital, was
admitted to Mosango General Hospital with a 5-
day history of fever, despite antimalarial
treatment. The day before hospitalization she
had profuse diarrhea, vomiting, high fever, and
severe agitation with delirium. On arrival, quiet
and apyretic, she complained of headache, loss of
appetite, and severe asthenia, but she walked to
her room without help. On examination, the only
abnormalities recorded were severe dehydration
and oral thrush-like lesions, raising a suspicion of
candidiasis. Pulse rate was 80/min and blood
pressure 120/80. Medical history included an
amebiasis liver abscess 15 years ago and chronic
coronaritis since 1990.
Electrocardiogram (ECG) abnormalities were
consistent with chronic diffuse ischemia. Laboratory
investigations showed the following values:
few trophozoites on a thick film; erythrocyte
sedimentation rate (ESR) 15 mm/h; bleeding time
(BT) 7½ min; coagulation time (CT) 9 min; and
white blood cells (WBC) 8.4x10
9/L (73% neutrophils,
23% lymphocytes, 2% eosinophils, 1%
basophils, 1% mastocytes). Urinalysis showed
proteinuria (++), hyaline cylinders (+++), 50
white cells per field, and hematuria (+). The
patient was perfused with 4L/day of glucose and
1.5 g of quinine. She was kept in a private room in
the nearby nuns’ convent.
Later during the day, high fever (40°C) and
severe diarrhea with melena developed; the pulse
rate was normal (80/min). Typhoid fever was
suspected despite the lack of hepatosplenomegaly;
Widal test was not available for
confirmation. Treatment was started with
intravenous (i.v.) amoxicillin (1g/6h during the
first 24 h and then 1g/4h) and i.v. chloramphenicol
(2g/24h). Subsequently, coagulation abnormalities
developed in addition to the melena;
vitamin K and epsilon amino caproic acid were
added to i.v. therapy. Watery vomits remained
frequent and abundant, and the patient’s
condition was unresponsive to treatment.
On hospitalization day 2, the clinical picture
remained the same, with severe asthenia,
anorexia, abundant blackish diarrhea, and
watery vomits. An intractable hiccup developed.
The fever remained in plateau around 40°C with
spikes. Obnubilation occurred during episodes of
high fever. Pulse and blood pressure remained
stable. ECG showed no modifications. Cutaneous
examination detected for the first time a
maculopapular rash and petechiae on flanks and
limbs, and the patient complained of gastric pain
for which the neurologic examination was
normal. Urine was abundant and clear.
On hospitalization day 3, high fever
continued, with some defervescence during
which the patient regained lucidity, although she
responded
only with monosyllables because of the
extreme asthenia and somnolence; diarrhea
persisted but without hemorrhage. The patient
had less vomiting. Laboratory data showed ESR
35 mm/h; BT 10 min; CT 12 min; WBC 12.6x10
9/L
(70% neutrophils, 24% lymphocytes, 2% eosinophils,
1% basophils, 3% mastocytes). During the
night, the patient maintained a high temperature,
still with temperature-pulse disparity. The
diagnosis of typhoid fever was questioned, and
other diagnostic possibilities were reconsidered
(shigellosis, mononucleosis); leukocytosis was
considered against the possibility of Ebola
hemorrhagic fever. Chloramphenicol was switched
to rifampicin (1,200 mg/24h).
On April 23, the patient’s status was
unchanged with fever, asthenia, and diarrhea.
Later in the day, her condition deteriorated:
petechiae could be seen on the entire body, and
for the first time, bruises and bleeding at
injection sites were observed and precluded
intramuscular injections. The patient had
bleeding cracks on the lips and diffuse bleeding in
the oral cavity (i.e., gums, tongue). The volume of
urine was low, and antibiotic therapy was
changed to cephalosporin.
On hospitalization day 5, hemorrhages increased,
and fever remained high until the end of
the day, when it started to normalize. Urine volume
was still low (verified by vesical catheter) despite
the i.v. rehydration of 4 L/day. Fresh blood
transfusion (300 ml) did not slow the hemorrhaging;
disseminated intravascular coagulation was
suspected, and heparin treatment was started.
The patient became comatose. The laboratory
results showed ESR 55mm/h and WBC 30.2x10
9/
L with an unchanged formula. No coagulation
was observed on BT and CT. Blood pressure fell
(80/50); the clinical status remained unchanged
until the patient’s death on April 25 at 10:00 a.m.
No special nursing precautions were taken
either during the hospitalization or after the
death, and the body was transferred to Kikwit to
be buried. On April 30, another nun who took care of
the index patient during the night of April 23
became ill with fever, headache, and myalgia. Over
the next few days, the second patient had a clinical
picture identical to that of the index patient,
including high fever, severe asthenia, vomiting,
hiccups, and diarrhea. On May 5, epistaxis and
coagulation abnormalities developed, followed by
other clinical signs of the hemorrhagic syndrome.
The second patient was transferred to Kikwit
General Hospital, where she died 6 days later. A
laboratory confirmation of Ebola hemorrhagic fever
was made on a blood specimen collected on May 5
and sent to Special Pathogens Branch (Centers for
Disease Control and Prevention, Atlanta, GA).
These cases of unrecognized Ebola hemorrhagic
fever were part of the hospital outbreak
that precipitated and mobilized international
community efforts (2). Retrospectively, the
clinical symptoms observed were typical of Ebola
hemorrhagic fever (3,4) and were described again
in subsequent patients during this outbreak (5).
In tropical Africa, the presence of hemorrhagic
symptoms in the course of a febrile illness should
raise the possibility of one of the viral hemorrhagic
fever diseases. In viral hemorrhagic fevers,
maculopapular rash is constantly observed only in
filovirus disease. Typically, the clinical laboratory
findings include an early lymphopenia and marked
thrombocytopenia. Containment and barrier nursing
procedures should be initiated until the
diagnosis of viral hemorrhagic fever can be ruled
out. The index patient described here was the third
patient transferred from Kikwit General Hospital
in less than 1 month to die of a hemorrhagic
illness after a few days of an unexplained febrile
syndrome. Two patients were health-care
workers in Kikwit General Hospital. This cluster
of hemorrhagic illness and possible human-tohuman
transmission, particularly among hospital
staff, was (and should always be) sufficient to
suspect a viral hemorrhagic fever. The laboratory
confirmation of this presumptive diagnosis was
the clenching factor in
he multinational effort in
Kikwit.
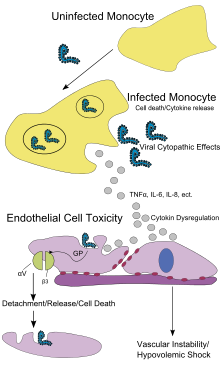 Endothelial cells, mononuclear phagocyte, and hepatocytes are the main targets of infection. After infection, in a secreted glycoprotein (sGP) the Ebola virus glycoprotein (GP) is synthesized. Ebola replication overwhelms protein synthesis of infected cells and host immune defenses. The GP forms a trimeric complex, which binds the virus to the endothelial cells lining the interior surface of blood vessels. The sGP forms a dimeric protein which interferes with the signaling of neutrophils, a type of white blood cell, which allows the virus to evade the immune system by inhibiting early steps of neutrophil activation. These white blood cells also serve as carriers to transport the virus throughout the entire body to places such as the lymph nodes, liver, lungs, and spleen. The presence of viral particles and cell damage resulting from budding causes the release of cytokines (specifically TNF-α, IL-6, IL-8, etc.), which are the signaling molecules for fever and inflammation. The cytopathic effect, from infection in the endothelial cells, results in a loss of vascular integrity. This loss in vascular integrity is furthered with synthesis of GP, which reduces specific integrins responsible for cell adhesion to the inter-cellular structure, and damage to the liver, which leads to coagulopathy.
Endothelial cells, mononuclear phagocyte, and hepatocytes are the main targets of infection. After infection, in a secreted glycoprotein (sGP) the Ebola virus glycoprotein (GP) is synthesized. Ebola replication overwhelms protein synthesis of infected cells and host immune defenses. The GP forms a trimeric complex, which binds the virus to the endothelial cells lining the interior surface of blood vessels. The sGP forms a dimeric protein which interferes with the signaling of neutrophils, a type of white blood cell, which allows the virus to evade the immune system by inhibiting early steps of neutrophil activation. These white blood cells also serve as carriers to transport the virus throughout the entire body to places such as the lymph nodes, liver, lungs, and spleen. The presence of viral particles and cell damage resulting from budding causes the release of cytokines (specifically TNF-α, IL-6, IL-8, etc.), which are the signaling molecules for fever and inflammation. The cytopathic effect, from infection in the endothelial cells, results in a loss of vascular integrity. This loss in vascular integrity is furthered with synthesis of GP, which reduces specific integrins responsible for cell adhesion to the inter-cellular structure, and damage to the liver, which leads to coagulopathy.
The most important indicator that may lead to the suspicion of EVD at clinical examination is the medical history of the patient, in particular the travel and occupational history (which countries were visited?) and the patient's exposure to wildlife (exposure to bats, bat excrement, nonhuman primates?). EVD can be confirmed by isolation of ebolaviruses from or by detection of ebolavirus antigen or genomic or subgenomic RNAs in patient blood or serum samples during the acute phase of EVD. Ebolavirus isolation is usually performed by inoculation of grivet kidney epithelial Vero E6 or MA-104 cell cultures or by inoculation of human adrenal carcinoma SW-13 cells, all of which react to infection with characteristic cytopathic effects. Filovirions can easily be visualized and identified in cell culture by electron microscopy due to their unique filamentous shapes, but electron microscopy cannot differentiate the various filoviruses alone despite some overall length differences.Immunofluorescence assays are used to confirm ebolavirus presence in cell cultures. During an outbreak, virus isolation and electron microscopy are most often not feasible options. The most common diagnostic methods are therefore RT-PCR in conjunction with antigen-capture ELISA which can be performed in field or mobile hospitals and laboratories. Indirect immunofluorescence assays (IFAs) are not used for diagnosis of EVD in the field anymore.
 Ebola viruses are highly infectious as well as contagious.
Ebola viruses are highly infectious as well as contagious.
As an outbreak of ebola progresses, bodily fluids from diarrhea, vomiting, and bleeding represent a hazard. Due to lack of proper equipment and hygienic practices, large-scale epidemics occur mostly in poor, isolated areas without modern hospitals or well-educated medical staff. Many areas where the infectious reservoir exists have just these characteristics. In such environments, all that can be done is to immediately cease all needle-sharing or use without adequate sterilization procedures, isolate patients, and observe strict barrier nursing procedures with the use of a medical-rated disposable face mask, gloves, goggles, and a gown at all times, strictly enforced for all medical personnel and visitors. The aim of all of these techniques is to avoid any person’s contact with the blood or secretions of any patient, including those who are deceased.
Vaccines have successfully protected nonhuman primates; however, the six months needed to complete immunization made it impractical in an epidemic. To resolve this, in 2003, a vaccine using an adenoviral (ADV) vector carrying the Ebola spike protein was tested on crab-eating macaques. The monkeys were challenged with the virus 28 days later, and remained resistant.In 2005, a vaccine based on attenuated recombinant vesicular stomatitis virus (VSV) vector carrying either the Ebola glycoprotein or Marburg glycoprotein successfully protected nonhuman primates, opening clinical trials in humans. By October, the study completed the first human trial; giving three vaccinations over three months showing capability of safely inducing an immune response. Individuals were followed for a year, and, in 2006, a study testing a faster-acting, single-shot vaccine began. This study was completed in 2008. The next step is to try the vaccine on a strain of Ebola that is closer to the one that infects humans.
There are currently no Food and Drug Administration-approved vaccines for the prevention of EVD. Many candidate vaccines have been developed and tested in various animal models. Of those, the most promising ones are DNA vaccines or are based on adenoviruses,vesicular stomatitis Indiana virus (VSIV)or filovirus-like particles (VLPs) as all of these candidates could protect nonhuman primates from ebolavirus-induced disease. DNA vaccines, adenovirus-based vaccines, and VSIV-based vaccines have entered clinical trials.
Contrary to popular belief, ebolaviruses are not transmitted by aerosol during natural EVD outbreaks. Due to the absence of an approved vaccine, prevention of EVD therefore relies predominantly on behavior modification, proper personal protective equipment, and sterilization/disinfection.
On 6 December 2011, the development of a successful vaccine against Ebola for mice was reported. Unlike the predecessors, it can be freeze-dried and thus stored for long periods in wait for an outbreak. The research will be presented in Proceedings of National Academy of Sciences.
Kikwit.
Virology
Main article: Ebola virus
Genome
Like all mononegaviruses, ebolavirions contain linear nonsegmented, single-stranded, non-infectious RNA genomes of negative polarity that possesses inverse-complementary 3' and 5' termini, do not possess a 5' cap, are not polyadenylated, and are not covalently linked to a protein. Ebolavirus genomes are approximately 19 kilobase pairs long and contain seven genes in the order 3'-UTR-NP-VP35-VP40-GP-VP30-VP24-L-5'-UTR.The genomes of the five different ebolaviruses (BDBV, EBOV, RESTV, SUDV, and TAFV) differ in sequence and the number and location of gene overlaps.Structure
Like all filoviruses, ebolavirions are filamentous particles that may appear in the shape of a shepherd's crook or in the shape of a "U" or a "6", and they may be coiled, toroid, or branched. Ebolavirions are generally 80 nm in width, but vary somewhat in length. In general, the median particle length of ebolaviruses ranges from 974–1,086 nm (in contrast to marburgvirions, whose median particle length was measured to be 795–828 nm), but particles as long as 14,000 nm have been detected in tissue culture. Ebolavirions consist of seven structural proteins. At the center is the helical ribonucleocapsid, which consists of the genomic RNA wrapped around a polymer of nucleoproteins (NP). Associated with the ribonucleoprotein is the RNA-dependent RNA polymerase (L) with the polymerase cofactor (VP35) and a transcription activator (VP30). The ribonucleoprotein is embedded in a matrix, formed by the major (VP40) and minor (VP24) matrix proteins. These particles are surrounded by a lipid membrane derived from the host cell membrane. The membrane anchors a glycoprotein (GP) that projects 7 to 10 nm spikes away from its surface. While nearly identical to marburgvirions in structure, ebolavirions are antigenically distinct.Replication
The ebolavirus life cycle begins with virion attachment to specific cell-surface receptors, followed by fusion of the virion envelope with cellular membranes and the concomitant release of the virus nucleocapsid into the cytosol. The viral RNA polymerase, encoded by the L gene, partially uncoats the nucleocapsid and transcribes the genes into positive-stranded mRNAs, which are then translated into structural and nonstructural proteins. Ebolavirus RNA polymerase (L) binds to a single promoter located at the 3' end of the genome. Transcription either terminates after a gene or continues to the next gene downstream. This means that genes close to the 3' end of the genome are transcribed in the greatest abundance, whereas those toward the 5' end are least likely to be transcribed. The gene order is therefore a simple but effective form of transcriptional regulation. The most abundant protein produced is the nucleoprotein, whose concentration in the cell determines when L switches from gene transcription to genome replication. Replication results in full-length, positive-stranded antigenomes that are in turn transcribed into negative-stranded virus progeny genome copy. Newly synthesized structural proteins and genomes self-assemble and accumulate near the inside of the cell membrane. Virions bud off from the cell, gaining their envelopes from the cellular membrane they bud from. The mature progeny particles then infect other cells to repeat the cycle.Pathophysiology
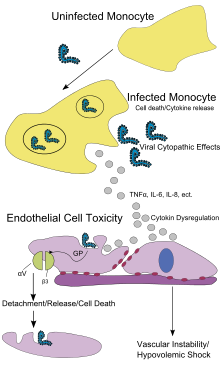
Pathogenesis schematic
Diagnosis
EVD is clinically indistinguishable from Marburg virus disease (MVD), and it can also easily be confused with many other diseases prevalent in Equatorial Africa, such as other viral hemorrhagic fevers, falciparum malaria, typhoid fever, shigellosis, rickettsial diseases such as typhus, cholera, gram-negative septicemia, borreliosis such as relapsing fever or EHEC enteritis. Other infectious diseases that ought to be included in the differential diagnosis include leptospirosis, scrub typhus, plague, Q fever, candidiasis, histoplasmosis, trypanosomiasis, visceral leishmaniasis, hemorrhagic smallpox, measles, and fulminant viral hepatitis. Non-infectious diseases that can be confused with EVD are acute promyelocytic leukemia, hemolytic uremic syndrome, snake envenomation, clotting factor deficiencies/platelet disorders, thrombotic thrombocytopenic purpura, hereditary hemorrhagic telangiectasia, Kawasaki disease, and even warfarin intoxication.The most important indicator that may lead to the suspicion of EVD at clinical examination is the medical history of the patient, in particular the travel and occupational history (which countries were visited?) and the patient's exposure to wildlife (exposure to bats, bat excrement, nonhuman primates?). EVD can be confirmed by isolation of ebolaviruses from or by detection of ebolavirus antigen or genomic or subgenomic RNAs in patient blood or serum samples during the acute phase of EVD. Ebolavirus isolation is usually performed by inoculation of grivet kidney epithelial Vero E6 or MA-104 cell cultures or by inoculation of human adrenal carcinoma SW-13 cells, all of which react to infection with characteristic cytopathic effects. Filovirions can easily be visualized and identified in cell culture by electron microscopy due to their unique filamentous shapes, but electron microscopy cannot differentiate the various filoviruses alone despite some overall length differences.Immunofluorescence assays are used to confirm ebolavirus presence in cell cultures. During an outbreak, virus isolation and electron microscopy are most often not feasible options. The most common diagnostic methods are therefore RT-PCR in conjunction with antigen-capture ELISA which can be performed in field or mobile hospitals and laboratories. Indirect immunofluorescence assays (IFAs) are not used for diagnosis of EVD in the field anymore.
Prevention

A researcher working with the Ebola virus while wearing a BSL-4 positive pressure suit to avoid infection
As an outbreak of ebola progresses, bodily fluids from diarrhea, vomiting, and bleeding represent a hazard. Due to lack of proper equipment and hygienic practices, large-scale epidemics occur mostly in poor, isolated areas without modern hospitals or well-educated medical staff. Many areas where the infectious reservoir exists have just these characteristics. In such environments, all that can be done is to immediately cease all needle-sharing or use without adequate sterilization procedures, isolate patients, and observe strict barrier nursing procedures with the use of a medical-rated disposable face mask, gloves, goggles, and a gown at all times, strictly enforced for all medical personnel and visitors. The aim of all of these techniques is to avoid any person’s contact with the blood or secretions of any patient, including those who are deceased.
Vaccines have successfully protected nonhuman primates; however, the six months needed to complete immunization made it impractical in an epidemic. To resolve this, in 2003, a vaccine using an adenoviral (ADV) vector carrying the Ebola spike protein was tested on crab-eating macaques. The monkeys were challenged with the virus 28 days later, and remained resistant.In 2005, a vaccine based on attenuated recombinant vesicular stomatitis virus (VSV) vector carrying either the Ebola glycoprotein or Marburg glycoprotein successfully protected nonhuman primates, opening clinical trials in humans. By October, the study completed the first human trial; giving three vaccinations over three months showing capability of safely inducing an immune response. Individuals were followed for a year, and, in 2006, a study testing a faster-acting, single-shot vaccine began. This study was completed in 2008. The next step is to try the vaccine on a strain of Ebola that is closer to the one that infects humans.
There are currently no Food and Drug Administration-approved vaccines for the prevention of EVD. Many candidate vaccines have been developed and tested in various animal models. Of those, the most promising ones are DNA vaccines or are based on adenoviruses,vesicular stomatitis Indiana virus (VSIV)or filovirus-like particles (VLPs) as all of these candidates could protect nonhuman primates from ebolavirus-induced disease. DNA vaccines, adenovirus-based vaccines, and VSIV-based vaccines have entered clinical trials.
Contrary to popular belief, ebolaviruses are not transmitted by aerosol during natural EVD outbreaks. Due to the absence of an approved vaccine, prevention of EVD therefore relies predominantly on behavior modification, proper personal protective equipment, and sterilization/disinfection.
On 6 December 2011, the development of a successful vaccine against Ebola for mice was reported. Unlike the predecessors, it can be freeze-dried and thus stored for long periods in wait for an outbreak. The research will be presented in Proceedings of National Academy of Sciences.





1 comment:
Organized content is the best way to display or post an article, thank you for making it easy to digest your
Digital Microscopes exporters india
Post a Comment